Patellar Tendinitis
Patellar tendinitis, It is reliably found in competitors, especially those pulled in with rehearses that require picked skipping, running, or abrupt heading shifts, like b-ball, volleyball, and soccer. In any case, it can similarly occur in individuals who partake in dismal activities that overburden the knee, such as cycling, running, or weightlifting. This article will explore the causes, symptoms, finding, treatment, and aversion frameworks for patellar tendinitis, helping individuals with sorting out this condition and regulate it, truth be told.
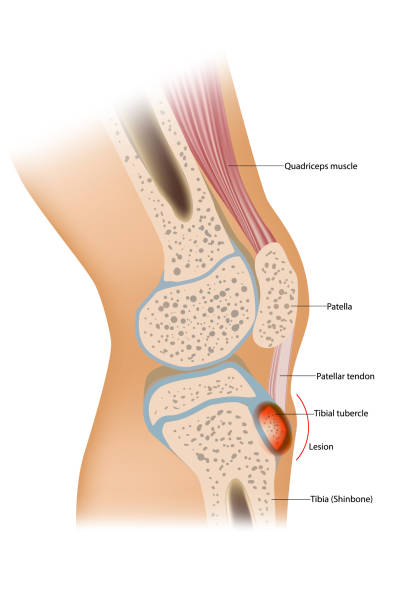
Life Anatomy of the Patellar Tendon
To comprehend patellar tendinitis, it is fundamental for first know the strategy of the patellar ligament. The patellar tendon is solid district for a, band of tissue that interfaces the lower part of the kneecap (patella) to the tibia, or shinbone. It assumes a basic part in the knee’s expansion system, considering legitimate development during exercises like standing, strolling, running, and hopping. The ligament works related to the quadriceps muscles, situated toward the front of the thigh, to take into consideration the knee to fix or broaden.
Causes of Patellar Tendinitis
Patellar tendinitis typically creates because of abuse or dreary burden on the patellar ligament, which causes little tears in the ligament strands. These tears lead to irritation and agony, which can slowly demolish over the long haul. A few variables add to the improvement of patellar tendinitis:
- Repetitive Jumping or Running: Activities that include redundant bouncing or running, especially with unexpected stops and starts, can overwhelm the patellar ligament. Competitors engaged with sports like ball, volleyball, and Olympic style events are more inclined to creating patellar tendinitis because of the successive hopping movements expected in these games.
- Overuse or Excessive Training: Overtraining or growing the force of dynamic work unnecessarily quick can cause the patellar tendon to become overemphasized. Consistently extending the power and repeat of action allows the tendon to change and avoid misuse wounds.
- Weak or Imbalanced Muscles: Weak quadriceps muscles or sporadic qualities in the muscles around the knee can add to patellar tendinitis. Exactly when the quadriceps are delicate, they can’t really maintain the knee joint, provoking excess weight on the patellar tendon. Tight or imbalanced muscles may similarly impact how the knee moves, further growing load on the tendon.
- Improper Footwear or Biomechanical Issues: Unfortunate footwear or irregularities in the arrangement and development examples of the legs, for example, level feet or unusual knee points, can modify how strain is appropriated during actual work. This can prompt expanded burden on the patellar ligament, eventually bringing about tendinitis.
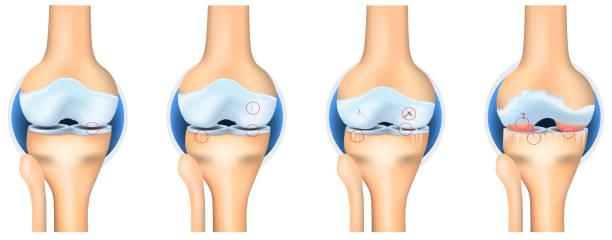
- Age and Degenerative Changes: As people age, the patellar ligament might lose a portion of its versatility and strength. This can make the ligament more helpless against injury, even with moderately low degrees of movement. More seasoned grown-ups may encounter patellar tendinitis because of these age-related changes.
Symptoms of Patellar Tendinitis
The primary symptom of patellar tendinitis is torment toward the front of the knee, especially close to the patellar ligament. The aggravation might start step by step and demolish over the long haul with proceeded with action. Other common symptoms include:
- Pain with Activity: People with patellar tendinitis frequently experience torment during exercises that include twisting or expanding the knee, like running, bouncing, hunching down, or climbing steps. The aggravation normally deteriorates with dreary utilization of the knee.
- Swelling and Tenderness: The region around the patellar ligament might become enlarged, and the actual ligament might feel delicate to the touch. The expanding might be more perceptible after movement or the next day.
- Stiffness: The knee might feel solid, especially after times of rest, and might be challenging to completely broaden or twist. This can restrict the scope of movement and cause inconvenience during ordinary developments.
- Pain at Rest: In further developed instances of patellar tendinitis, torment might happen in any event, when the individual isn’t taking part in active work, particularly after delayed times of rest or dormancy.
- Weakness in the Knee: As the condition advances, shortcoming in the knee might create, making it challenging to play out specific developments, for example, standing up from a situated position or strolling for broadened periods.
Diagnosis of Patellar Tendinitis
Diagnosing patellar tendinitis typically includes a mix of an actual assessment, clinical history survey, and imaging tests. The clinical benefits provider will overview the patient’s secondary effects and may perform express tests to evaluate the capacity of the knee and the patellar tendon.
- Physical Examination: The doctor will survey the knee for indications of delicacy, expanding, and limited development. They may likewise check for agony and shortcoming during exercises that include knee expansion, like crouching or hopping.
- Medical History: The specialist will get some information about the patient’s activity levels, the start and development of secondary effects, and any previous injuries or conditions that may be adding to the issue.
- Imaging Tests: on occasion, the specialist could recommend imaging tests like X-pillars, ultrasound, or alluring resonation imaging (X-beam) to assess the condition of the patellar tendon. While X-radiates don’t show sensitive tissue wounds, they may be used to block various conditions, similar to breaks or joint aggravation. Ultrasound or X-pillar can give point by point photographs of the patellar ligament, permitting the master to evaluate the degree of harm or unsettling influence.
Treatment for Patellar Tendinitis
The treatment of patellar tendinitis expects to reduce torture, advance patching, and restore capacity to the knee. Most occurrences of patellar tendinitis can be managed securely with rest and recuperation. Normal treatment choices include:
- Rest and Activity Modification: The most important phase in treating patellar tendinitis is to diminish or adjust exercises that disturb the condition. This might include briefly keeping away from exercises, for example, bouncing or running that overwhelm the knee. Low-influence works out, like swimming or cycling, might be suggested as options.
- Ice Therapy: Applying ice to the knee can assist with diminishing irritation and reduce torment. Ice should be applied for 15-20 minutes at the same time, a couple of times every day, particularly after genuine work.
- Anti-fiery Medications: Nonsteroidal moderating medications (NSAIDs), like ibuprofen or naproxen, may be used to diminish misery and bothering. These drugs should be taken as composed and should not be relied on long stretch.
- Physical Therapy: A Physical specialist can plan a recovery program to work on the strength and adaptability of the muscles encompassing the knee. Extending and reinforcing practices for the quadriceps, hamstrings, and lower leg muscles can assist with decreasing burden on the patellar ligament and forestall further injury. Unusual activities, in which the muscle is stretched while under pressure, are especially successful for treating tendinitis.
- Knee Bracing or Taping: Using a patellar ligament tie or support can assist with diminishing stress on the ligament during action. Taping techniques, for instance, McConnell taping, may similarly give temporary assistance by changing the arranging of the patella and revising weight on the tendon.
- Corticosteroid Injections: at times, a specialist might prescribe a corticosteroid infusion to diminish irritation and ease torment. Regardless, corticosteroid mixtures should be used with alert, as they can cripple the tendon over an extended time and augmentation the bet of burst at whatever point used too constantly.
- Surgical Treatment: In uncommon situations where moderate medicines don’t give help, medical procedure might be vital. Careful choices might include eliminating harmed tissue or fixing the ligament. Medical procedure is regularly saved for people with constant or serious tendinitis that doesn’t answer different therapies.
Prevention of Patellar Tendinitis
Preventing patellar tendinitis involves minimizing the risk factors that contribute to the development of the condition. A few procedures can assist with forestalling abuse wounds and safeguard the patellar ligament:
- Warm-Up and Stretching: Appropriately heating up before actual work and extending the muscles around the knee can assist with forestalling injury. Base on broadening the quadriceps, hamstrings, calves, and hip flexors to maintain with flexibility and abatement tension on the knee joint.
- Strengthening Exercises: Building up the muscles around the knee, particularly the quadriceps, can help with supporting the patellar tendon and diminishing strain. Consolidate activities like squats, thrusts, and leg presses into your gym routine daily practice.
- Gradual Progression: Keep away from abrupt expansions in the force or term of active work. Progressively develop your preparation routine to give your body time to adjust and diminish the gamble of abuse wounds.
- Proper Footwear: Wear steady shoes that offer appropriate curve help and padding. Pick footwear that is fitting for the action you are performing, as ill-advised shoes can add to knee strain.
- Cross-Training: Integrating various exercises into your exercise routine can assist with forestalling abuse wounds by lessening tedious stress on the knee. Consider switching back and forth between low-influence works out, like swimming or cycling, and higher-influence exercises.
Conclusion
Patellar tendinitis is a common condition that can affect individuals who engage in activities involving repetitive knee stress, such as jumping and running. While the condition can cause critical agony and inconvenience, it is for the most part treatable with rest, active recuperation, and other moderate measures. By figuring out the causes, side effects, and treatment choices for patellar tendinitis, people can do whatever it takes to actually forestall and deal with the condition. With proper consideration and restoration, a great many people with patellar tendinitis can get back to their customary exercises without long haul entanglements.
[sp_easyaccordion id=”4676″]

Dr. Hamza is a medical content reviewer with over 12+ years of experience in healthcare research and patient education. He specializes in evidence-based health information, medications, and chronic conditions. His reviews are grounded in trusted medical sources and current clinical guidelines to ensure accuracy, transparency, and reliability. Content reviewed by Dr. Hamza is intended for educational purposes and is not a substitute for professional medical advice.
