Treatment Guidelines
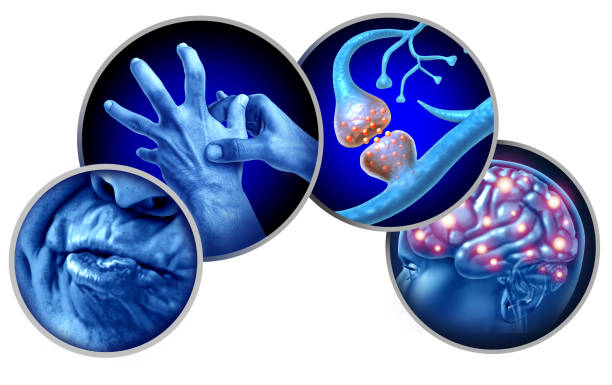
Tardive dyskinesia Treatment Guidelines (TDTG) is a neurological problem portrayed by compulsory, dreary developments, generally impacting the face, tongue, lips, and at times the members or trunk. This condition much of the time makes because of long stretch usage of dopamine receptor-ruining solutions, particularly antipsychotics. With the rising utilization of these prescriptions to oversee mental problems, it is fundamental to lay out far reaching treatment rules to oversee and moderate the side effects of TD successfully. These rules mean to give an organized way to deal with finding, treatment, and long haul the executives, improving the personal satisfaction for patients impacted by this condition.
Diagnosis of Tardive Dyskinesia
The accurate diagnosis of TD is critical for appropriate treatment and management. It includes a nitty gritty clinical evaluation and the prohibition of other development issues. Key stages in diagnosing TD include:
- Patient History: A careful clinical history is fundamental, zeroing in on the term and sort of dopamine receptor-hindering meds utilized. It is additionally vital to evaluate the course of events of side effect beginning comparative with prescription use.
- Clinical Examination: Perception of compulsory developments during rest and different exercises is essential. The Unusual Compulsory Development Scale (Points) is a generally involved instrument for surveying the seriousness and recurrence of TD side effects.
- Differential Diagnosis: Other development issues, like Parkinson’s illness, dystonia, and Huntington’s infection, ought to be precluded. This might include neuroimaging or other indicative tests depending on the situation.
- Monitoring: Normal subsequent appraisals are prescribed to follow the movement of side effects and the effect of treatment mediations.

Treatment Guidelines for Tardive Dyskinesia
Effective management of TD requires a multifaceted approach, zeroing in on both side effect control and the basic causes. The accompanying treatment rules are suggested:
1. Medication Review and Adjustment
The most important phase in overseeing TD is to assess the patient’s ongoing drug routine:
- Lessen or Suspend Irritating Medications: If clinically possible, decreasing the portion or ending the utilization of the medicine causing TD might assist with diminishing side effects. Nonetheless, this should be adjusted against the gamble of worsening the fundamental mental condition.
- Changing Medications: Progressing from an original (common) antipsychotic to a second-age (abnormal) antipsychotic, which has a lower hazard of causing TD, might be useful. Among abnormal antipsychotics, clozapine has shown minimal relationship with TD.
2. Use of VMAT2 Inhibitors
VMAT2 (vesicular monoamine transporter 2) inhibitors have arisen as successful medicines for TD:
- Valbenazine and Deutetrabenazine: These prescriptions are FDA-supported for the treatment of TD. They work by decreasing the arrival of dopamine in the cerebrum, in this way easing the compulsory developments related with TD. These medications have been displayed to further develop side effects essentially and are by and large all around endured.
- Dose and Monitoring: The dosing of VMAT2 inhibitors ought to be individualized in light of the seriousness of side effects and patient reaction. Normal observing for secondary effects, like sedation and sorrow, is suggested.
3. Symptomatic Treatment Options
In situations where VMAT2 inhibitors are not reasonable or extra side effect control is required, different meds might be thought of:
- Benzodiazepines: Medications like clonazepam can assist with decreasing muscle fits and uneasiness related with TD. Be that as it may, their utilization ought to be restricted because of the gamble of reliance.
- Anticholinergic Agents: These prescriptions can assist with reducing a few engine side effects yet may compound mental incidental effects, especially in more seasoned grown-ups.
- Beta-Blockers: Propranolol might be helpful in overseeing quakes and other engine side effects in certain patients.
4. Non-Pharmacological Interventions
Strong treatments assume a pivotal part in the thorough administration of TD:
- Actual Therapy: Customized activities can assist with working on engine control and decrease the effect of TD on day to day exercises.
- Word related Therapy: Methodologies to adjust errands and conditions can upgrade freedom and personal satisfaction.
- Discourse Therapy: For patients with discourse and gulping troubles, language instruction can give important methods to deal with these difficulties.
5. Psychosocial Support
Living with TD can fundamentally influence a patient’s psychological wellness and social connections:
- Directing and Backing Groups: Offering profound help through advising and uphold gatherings can assist patients with adapting to the mental weight of TD.
- Education: Teaching patients and their families about TD, its causes, and the executives systems is fundamental for enabling them to play a functioning job in their consideration.
6. Regular Monitoring and Follow-Up
Consistent observing is essential for surveying treatment adequacy and changing the administration plan on a case by case basis:
- Ordinary Utilization of AIMS: Occasional evaluations utilizing apparatuses like the Points can assist with following side effect changes and the effect of mediations.
- Patient-Revealed Outcomes: Empowering patients to report changes in side effects and aftereffects can direct treatment changes.

7. Prevention Strategies
Forestalling the beginning of TD is a basic part of the board, particularly for patients requiring long haul antipsychotic treatment:
- Risk Assessment: Consistently evaluate the gamble of TD in patients on antipsychotic treatment, particularly those on high portions or with delayed use.
- Limiting Exposure: Utilize the least successful portion of antipsychotics for the most brief length important to oversee mental side effects.
- Early Detection: Execute routine evaluating for early indications of TD, especially in high-risk populaces like more established grown-ups and ladies.
8. Emerging Therapies and Research
Continuous investigation into TD is cantered around understanding its pathophysiology and growing new medicines:
- Neuroprotective Agents: Examining specialists that might safeguard against the neurotoxic impacts of dopamine receptor bar.
- Quality Therapy: Investigating the potential for quality based mediations to address fundamental hereditary weaknesses related with TD.
- Novel Pharmacological Approaches: Growing new medications that target various pathways engaged with TD pathogenesis.
Conclusion
The management of tardive dyskinesia requires a comprehensive and individualized approach, adjusting the requirement for viable mental treatment with the minimization of TD side effects. Early identification, ordinary observing, and the utilization of proof based intercessions, including VMAT2 inhibitors and steady treatments, are critical for further developing results. Deterrent techniques and continuous examination into new medicines hold guarantee for lessening the weight of TD later on. By complying with these treatment rules, medical services suppliers can advance consideration for patients with TD, enhancing their quality of life and overall well-being.
[sp_easyaccordion id=”4330″]

Dr. Hamza is a medical content reviewer with over 12+ years of experience in healthcare research and patient education. He specializes in evidence-based health information, medications, and chronic conditions. His reviews are grounded in trusted medical sources and current clinical guidelines to ensure accuracy, transparency, and reliability. Content reviewed by Dr. Hamza is intended for educational purposes and is not a substitute for professional medical advice.